STREAMLINE PROCESSES
IMPROVE PATIENT OUTCOMES
REDUCE OVERALL RISK
Stop Stalling Due to Inefficiencies
Struggling to keep up with the ever-changing market?
Overwhelmed with complex yet ineffective technology?
Unable to manage operational costs?
Optimize Your Accuracy, Time & Costs
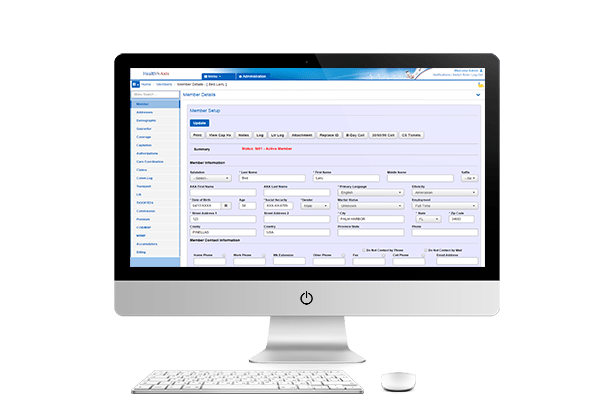
HealthAxis equips payers, risk-bearing providers, and health organizations with integrated solutions from an advanced claims system to TPA services.
Through our tech-enabled services, health plan organizations can provide enhanced member services, adapt quickly, offer new products to members, and improve outcomes, all while reducing overall risk.

A Claims Management Partner
When you work with HealthAxis you’re not just getting new software, you are getting partners.
There’s nothing worse than being onboarded as a client only to get ghosted by your software support. Our customer support is always here to answer your questions using our expertise in various sectors throughout the healthcare landscape.
A comprehensive healthcare claims processing system built for your business
Want to work with us?
To see our solutions in action, let’s get started with your information.


