Dedicated to Driving Operational Excellence
Whether it’s through outsourcing critical business processes, augmenting your staff with expert talent, or providing strategic consulting, HealthAxis is committed to driving operational excellence in every aspect of your business.
HealthAxis by the Numbers
0
Years of Experience$0B+
Claims Paid Annually0M+
Claims Processed Annually0+
Health Plans Served0+
Benefits Plans Managed
Unmatched Advantages: Elevating Your Operations
See What Our Clients Are Saying
Learn More About Our Comprehensive Suite of Tech and Services
Pair our experts with best-in-breed technology and services designed to maximize operational efficiency and elevate the member experience.
Core Admin Tech
Leverage our modern CAPS platform designed to enhance crucial human interactions, optimizing efficiency and improving service quality in key administrative areas.
Consulting
Harness our expertise in core system optimization, contact center augmentation, and compliance adherence, for tailored solutions across all plan types.
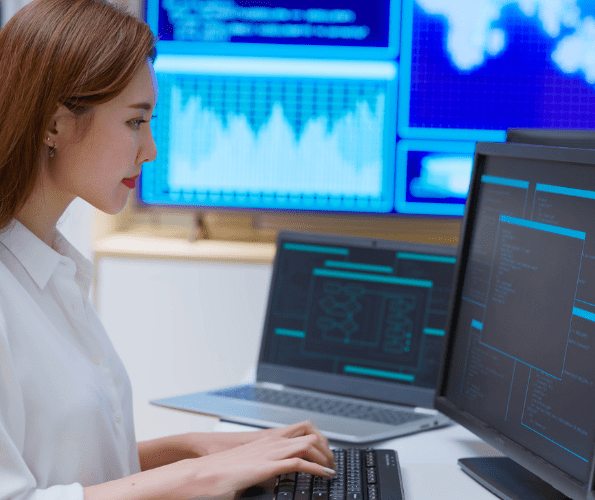
Staff Augmentation
Gain instant access to our deep bench of operational resources. We can deploy on-demand, top-tier talent to support your claims, enrollment, IT, and contact center labor needs.